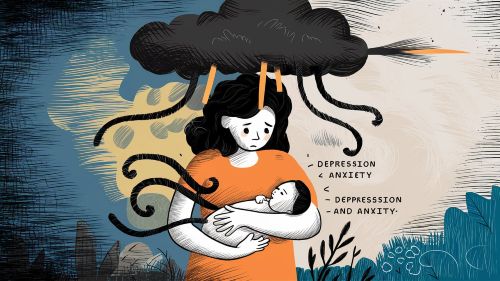
You were prepared for the possibility of postpartum depression. You’d read about the persistent sadness, the numbness, the heavy fog that can settle after childbirth. Or perhaps you were braced for postpartum anxiety—the frantic, heart-pounding worry that something terrible is about to happen to your baby.
But what if what you’re feeling isn’t one or the other?
What if it’s both?
What if your days are a confusing, exhausting cocktail of emotions? One moment, your mind is racing with terrifying “what-if” scenarios, and the next, you’re so weighed down by despair you can barely get out of bed. You feel wired and tired, agitated and empty, panicked and numb—all at the same time.
If this describes your reality, you are not losing your mind. You are experiencing the most common, yet least-discussed, aspect of postpartum mental health: the profound and intricate overlap of depression and anxiety.
These conditions are not neat, separate boxes. For most new mothers, they are a tangled knot of symptoms, thoughts, and feelings. In this article, we will gently pull on those threads to understand how and why they intertwine, what this overlap feels like, and why seeing the full picture is the most important step toward getting well.
[Insert a compelling, metaphorical image here: a tangled ball of yarn, two different colored threads twisted together, or intertwined roots of a tree.]
Moving Beyond Separate Boxes: Welcome to PMADs
In our last article, we drew a clear line between Postpartum Anxiety (PPA) and Postpartum Depression (PPD). This is a crucial first step. To recap briefly:
- Postpartum Depression (PPD) is primarily defined by sadness, hopelessness, and a loss of joy (anhedonia). It’s a heavy, draining weight.
- Postpartum Anxiety (PPA) is primarily defined by fear, worry, and a sense of dread. It’s a frantic, activating energy.
But in the real world, the line between them blurs. That’s why mental health professionals increasingly use the umbrella term Perinatal Mood and Anxiety Disorders (PMADs). This term acknowledges that after birth, women can experience a whole spectrum of symptoms, and that anxiety and depression are often two sides of the same coin.
Research confirms this. According to the National Institute of Mental Health (NIMH), up to 50% of those with PPD also have a co-existing anxiety disorder. They are partners in crime, and understanding their toxic teamwork is key to dismantling their power.
The Vicious Cycle: How Anxiety and Depression Fuel Each Other
The overlap isn’t just a coincidence; it’s a dynamic, self-perpetuating cycle. Anxiety can directly lead to depression, and depression can just as easily trigger anxiety. Let’s break down this feedback loop.
Path 1: How Unchecked Anxiety Spirals into Depression
Imagine your postpartum experience starts with anxiety. Your mind is a whirlwind of worry. Is the baby breathing? Am I producing enough milk? What if I trip on the stairs while holding her?
- Constant Hyper-Vigilance: Your body is flooded with stress hormones like adrenaline and cortisol. You’re always “on,” unable to relax.
- Mental and Physical Exhaustion: This state of high alert is not sustainable. It’s like running a mental marathon every single day. You become profoundly exhausted, but your racing mind prevents restorative sleep.
- Feeling Overwhelmed and Out of Control: Despite your best efforts to control everything, the anxiety persists. You start to feel powerless against your own thoughts.
- Hopelessness and Withdrawal: The exhaustion and feeling of powerlessness lead to hopelessness. You think, “I can’t live like this. It’s never going to stop.” This despair is the gateway to depression. You lose interest in things because you simply don’t have the mental or physical energy for them.
- The Crash: The frantic energy of anxiety burns itself out, leaving behind the hollowed-out emptiness of depression.
In short: Relentless fear → Exhaustion → Hopelessness → Depression.
Path 2: How the Weight of Depression Creates Anxiety
Now, let’s imagine the journey starts with depression. You feel numb, disconnected from your baby, and weighed down by a sadness you can’t explain.
- Guilt and Shame: You look at your baby and feel… nothing. Or worse, you feel resentment. This is immediately followed by a crushing wave of guilt. “What kind of mother feels this way? I am a terrible person.”
- Fear of Inadequacy: This guilt morphs into anxiety. You become anxious about your ability to care for your baby properly. You worry that your depression is harming your child or that you will never bond with them.
- Anxiety About the Depression Itself: You become terrified of the depression. “What if I feel like this forever? What if I never get better? What if I’m losing my mind?” This fear about your mental state is a form of anxiety.
- Physical Symptoms of Panic: The intense fear can trigger the physical symptoms of anxiety—a racing heart, shortness of breath, a feeling of panic—layering on top of the depressive lethargy.
In short: Numbness and Sadness → Guilt and Shame → Fear of Failure → Anxiety.
[WordPress Tip: Use the “Columns” block to create a simple visual flowchart for these two paths. For example, in a two-column layout: Left column has “Anxiety” with an arrow pointing to the right column, which has “Exhaustion & Hopelessness,” with another arrow pointing to “Depression.” Do the same for the second path.]
Shared Roots: The Common Triggers for Both Conditions
Anxiety and depression don’t just fuel each other; they often grow from the same soil. Several powerful biological and situational factors in the postpartum period can trigger both conditions simultaneously.
The Biological Bedrock
- The Hormone Plunge: After you deliver the placenta, levels of estrogen and progesterone—which were at all-time highs during pregnancy—plummet dramatically within hours. These hormones are powerful mood regulators. This sudden withdrawal can destabilize the brain’s entire chemical balance, impacting neurotransmitters like serotonin (linked to depression) and GABA (linked to anxiety), leaving you vulnerable to both.
- The HPA-Axis (Your Stress System): The Hypothalamic-Pituitary-Adrenal axis is your body’s central stress response system. The immense stress of childbirth, recovery, and round-the-clock infant care can throw this system into overdrive. A dysregulated HPA-axis can lead to both the “fight-or-flight” feelings of anxiety (too much cortisol at the wrong times) and the “burnout” and fatigue of depression (the system becoming exhausted).
- Sleep Deprivation: This is perhaps the single greatest contributor. Chronic sleep deprivation is used as a form of torture for a reason. It severely impacts the prefrontal cortex—the part of your brain responsible for emotional regulation, rational thought, and decision-making. Without it, your brain’s more primitive fear center (the amygdala) runs wild, breeding anxiety, while your capacity for positive emotion and motivation plummets, causing depression.
The Situational Storm
- Loss of Identity and Control: The transition to motherhood is a monumental identity shift. You may grieve your old life, freedom, and sense of self (leading to depression), while also feeling intense fear and uncertainty about your new role and responsibilities (leading to anxiety).
- Isolation: Modern motherhood can be incredibly lonely. Being home all day with a non-verbal infant, disconnected from colleagues and friends, creates a perfect breeding ground for both depressive rumination and anxious, circular thinking.
- Societal Pressure: The unrealistic expectation to be a “perfect,” blissful new mother creates immense pressure. When your reality doesn’t match this ideal, it can lead to feelings of failure and shame (depression) and a frantic anxiety to try and “get it right.”
A Story of the Tangled Knot
“For the first few months, I felt like two different people at war inside my own head. In the daytime, I would be paralyzed by depression. I’d sit on the couch, unable to muster the energy to shower, feeling this deep, hollow ache inside me. I felt no joy, just a profound sense of failure.
But at night, anxiety took over. As soon as my head hit the pillow, my heart would start pounding. My brain would serve up one horrific image after another—the baby falling, the car crashing, a house fire. I’d get up and check on her a dozen times. I was so exhausted from the depression, but so wired from the anxiety. It was a special kind of hell. I didn’t know what to call it until a therapist told me, ‘It’s both. You have both.’ Hearing that was the first time I felt sane in months.”
— Chloe, a mom of twins
[Use the WordPress “Quote” block to highlight this powerful, relatable story.]
What the Overlap Feels Like: Blended Symptoms
When PPD and PPA are intertwined, they create unique, blended symptoms that can be especially confusing.
- Rage and Irritability: Is your sudden snap of anger from the low frustration tolerance of depression, or the feeling of being overwhelmed and on-edge from anxiety? It’s both. The exhaustion of depression lowers your fuse, and the hyper-arousal of anxiety provides the explosive spark.
- Complex Sleep Issues: You experience the classic “wired but tired” phenomenon. You desperately crave sleep due to depressive fatigue, but when you lie down, your anxious, racing mind won’t let you have it.
- Intrusive Thoughts with a Double-Punch: Anxiety or Postpartum OCD provides the horrific, unwanted thought or image (e.g., of the baby getting hurt). Depression immediately follows up with a wave of shame and self-loathing for having had such a “terrible” thought in the first place.
- Paralyzed Avoidance: You might avoid taking the baby to the grocery store. Is it because you lack the energy and motivation (depression), or because you’re terrified of the baby catching germs or having a meltdown in public (anxiety)? For many, it’s a crippling combination of both.
[Insert an image here showing a woman looking exhausted and stressed, sitting on a couch in a messy room, to represent the feeling of being overwhelmed.]
Why This Matters: A Roadmap for Comprehensive Treatment
Understanding that you likely have a comorbid condition isn’t meant to be a scarier diagnosis. It’s a more accurate one. And accuracy is power. It tells you and your healthcare provider that you need a treatment plan that addresses the whole, tangled picture.
Fortunately, the frontline treatments for PPD and PPA are highly effective for the overlap.
- Integrated Therapy: A good therapist specializing in PMADs will not treat your anxiety and depression separately. They will use an integrated approach. For example, using Cognitive Behavioral Therapy (CBT), they can help you:
- Challenge the catastrophic “what if” thoughts of anxiety.
- And simultaneously challenge the self-defeating “I am a failure” thoughts of depression.
- Teach you grounding techniques to calm panic attacks (for anxiety) and behavioral activation strategies to fight lethargy (for depression).
- Effective Medication: This is where the overlap is actually good news. The most commonly prescribed class of medications, SSRIs (Selective Serotonin Reuptake Inhibitors), are highly effective at treating both anxiety and depression. By regulating serotonin, they can simultaneously lift the weight of depression and calm the storm of anxiety.
- Holistic Support: Strategies that regulate the nervous system help the entire system.
- Prioritizing sleep calms the anxious brain and restores energy to the depressed body.
- Gentle movement burns off anxious adrenaline and releases mood-boosting endorphins.
- Proper nutrition stabilizes blood sugar, preventing crashes that worsen both conditions.

Frequently Asked Questions (FAQ)
Q1: Does having both PPD and PPA mean my condition is more severe?
Not necessarily, but it does mean your experience is more complex. The good news is that treatment is designed to handle this complexity. Recognizing the overlap simply allows for a more targeted and comprehensive recovery plan.
Q2: If my anxiety gets better with treatment, will my depression go away too?
Often, yes. Since the two are so intertwined, reducing the exhausting burden of anxiety can free up mental and emotional resources, which helps lift the depression. Similarly, as depression lifts and you regain energy and hope, your anxiety about your mental state will also decrease. A good treatment plan addresses both simultaneously.
Q3: How do I explain this “mixed” feeling to my doctor?
You don’t need the perfect words. Be honest about the confusion. You can use phrases like:
- “I feel both incredibly anxious and incredibly sad.”
- “My mind is always racing with worry, but my body feels heavy and exhausted.”
- “I have no motivation, but I can’t relax.”
A good provider will hear these “contradictions” and immediately recognize the classic PPD/PPA overlap.
Untangling the Knot, One Thread at a Time
If you have been feeling at war with yourself, trapped between the frantic energy of fear and the crushing weight of despair, please know this: you are not broken. You are experiencing the common, tangled reality of a postpartum mood and anxiety disorder.
Seeing this overlap is not a cause for more fear. It is a cause for compassion for yourself. It is the map that shows you’re not lost in two separate woods, but navigating one complex forest.
The journey out is not about yanking on the knot and hoping it comes undone. It’s about seeking the right tools—therapy, medication, support—and gently, patiently, untangling one thread at a time. The fear will subside. The sadness will lift. And in the space that’s left, you will find peace, you will find joy, and you will find yourself again.
